?We do ourselves a disservice when diagnoses as wildly different as a?grade 4 glioblastoma multiforme?(a brain tumour that is virtually 100% fatal) and?prostatic intraepithelial neoplasia?(a prostate condition more likely to make you pee frequently than to kill you) are both described as?cancer.?
So claims a thoughtful?Globe and Mail?reflection called?Can the Word ?Cancer? Be More Harmful Than the Disease??by health columnist?Andr? Picard. It?s all about the power of words ? and particularly the C-word.
We know that not all tumours in the body are cancerous, Picard reminds us.? Tumours can be?malignant?(spreading to other parts of the body) or?benign?(they do not spread). Some cancers, like leukemia, do not even form tumours at all.
?We can now detect tumours at a microscopic level and abnormalities right down to a cellular level ? and we can do this in living people. For the longest time, cancer was studied only in corpses, reinforcing cancer?s deadly reputation.
?The paradox is that we can now detect a lot of cancer that is not even cancer yet,?and likely never will be.
?Should we be telling folks with abnormalities or weird-looking cells that they have cancer??
That?s also the??bombshell??dropped at a recent National Institutes of Health?Consensus Development Panel?meeting, as?described?by?Reporting On Health?s?Laura Newman. Members of the Panel on?active surveillance for prostate cancer?made a sweeping recommendation about when doctors should actually say the C-word out loud to their prostate patients.
The panel members insist that??terminology matters?,?and that men who have prostate-specific antigen (PSA) screening results that read?10?nano-grams?(ngs)or less?with a Gleason Score of 6 or less?should no longer be told that they have prostate??cancer.?
According to the National Cancer Institute, most doctors in the past?considered a PSA levelbelow 4.0 ng/mL?as normal. But in a number of studies, PSA measurements?above 2.5-3.0 ng?have been considered??elevated?.? These lower cutoff levels may increase the chance of detecting prostate cancer, but the reality is that this method also?increases overdiagnosis and false-positive test results, leading to unnecessary and debilitating medical procedures.
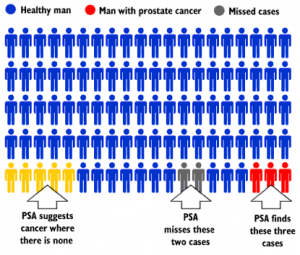
The PSA screening test itself has become controversial.?(See Health Canada?s infographic above).?For example, two large, randomized clinical trials in 2009 studied the relationship between PSA-based screening and prostate cancer mortality:
- The?European Randomized Study of Screening for Prostate Cancer
- ?The?Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial? (U.S.A.)
According to the?European study, which involved over 162,000 men between the ages of 50 and 74 in seven countries, PSA-based screening reduced the already low rate of death from prostate cancer, but was also?associated with a?high risk of overdiagnosis and overtreatment?leading to devastating quality-of-life consequences like incontinence and impotence ? often permanent.
Meanwhile, the?American PLCO study?found the rate of death from prostate cancer was very low for both the 38,343 men in the group that received annual PSA-based screening and the 38,350 men in the control group who received??usual care.?? The conclusion:
?Screening was associated with no reduction in prostate cancer mortality.?
In fact, as?Dr. Richard J. Ablin, the inventor of the PSA test, wrote in the?New York Times:
?Men lucky enough to reach old age are much more likely to die?with?prostate cancer than to die?because?of it.?
A December 2011 editorial in the?British Journal of Urology International?also stated:
?There is no doubt that prostate cancer kills, but only a minority of men who are given this diagnosis, die from prostate cancer. In the developed world, we are now over-diagnosing and, more importantly, overtreating prostate cancer, a fact for which we will be criticized in generations to come.?
According to veteran urologist?Dr. Anthony Horan, author of?The Big Scare: The Business of Prostate Cancer, 94% of the cancers detected with the routine PSA blood test would not cause death before the age of 85.
?More men die in car accidents than of prostate cancer each year.?
The medical profession is already familiar with the accepted practice of renaming certain cancer diagnoses, based on evolving scientific knowledge.
For example, consider the?Globe and Mail?s update on the changing distinctions for these forms of skin, breast, cervical and thyroid??cancers.?
- The Canadian Cancer Society does not count the 74,100?non-melanoma?skin cancers?in its annual tally of cancer diagnoses in Canada because these are considered just??localized abnormalities?.
- Ductal Carcinoma In Situ?(DCIS), also known as?Stage Zero breast cancer, is an accumulation of abnormal-looking cells in the milk ducts of the breast, accounting for?one in five cases of breast cancer. But is it actually cancer at all? While DCIS can spread from the milk ducts to elsewhere, there is no good science showing that treating it before it spreads is beneficial, and the U.S. National Institutes of Health have concluded that?DCIS is?not a carcinoma, so it should be renamed??high-grade dysplasia.?
- Cervical carcinoma in situ?has already been renamed?cervical intraepithelial neoplasia?? not a form of cancer. Women understand that an abnormal Pap test does?not?automatically mean they have cancer; they already make the distinction between dysplasia and cancer.
- The fastest-growing cancer here in Canada is?thyroid cancer. But, again, is that misleading? As with DCIS, we now have technology that can detect nodules on the thyroid. But the vast majority are benign ? and they will have no negative health consequence,?unless you start cutting them out.
Finally, as the?Globe and Mail?s?Andr? Picard sums up the power of words:
?When you use the dreaded C-word,? the reaction of patients is to want to rid their body of a deadly passenger. They want to cut it out ? whether it?s in a breast, a prostate or a thyroid. But cutting and burning and poisoning ? surgery, radiation and chemotherapy if you prefer the more technical terms ? are not always the best response to weird-looking cells.
?Watchful waiting is becoming an increasingly common practice, particularly with prostate cancer, where the screening test (PSA or prostate specific antigen) is notoriously poor and tumour growth often very slow.?
Reproduced with permission from The Ethical Nag: marketing Ethics for the Easily Swayed by Carolyn Thomas -?? http://ethicalnag.org Carolyn has over 37 years experience in journalism marketing and public relations.She has a particular interest in medical research and Big Pharma marketing issues.
The original article appears here
Tags: breast cancer, cancer screening, Carolyn Thomas, prostate cancer, prostate screening, screening tests
Source: http://www.drjoetoday.com/should-we-stop-calling-it-prostate-cancer/
weather radar aapl broncos broncos lehigh walking dead season finale aubrey o day
No comments:
Post a Comment